March Health Care News Roundup
Here are the top news stories on the health care system and the right to health in March. This is an excerpt from the most recent edition of the Healthcare Is a Human Right News Bulletin, a monthly enewsletter that features updates from Healthcare Is a Human Right campaigns for universal, publicly financed health care.
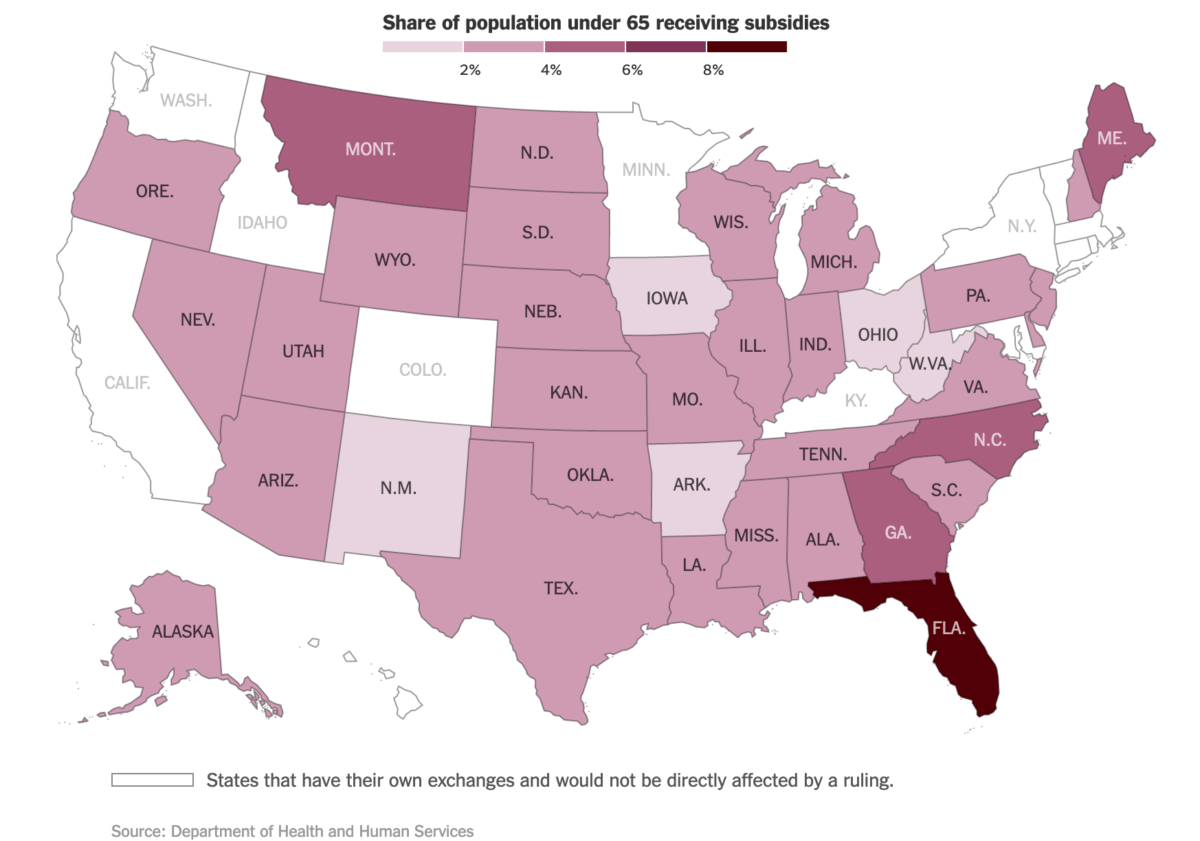
The Supreme Court Challenge to the ACA: The Supreme Court heard oral arguments the first week of March in King v. Burwell, the court case questioning whether the Affordable Care Act grants the federal government authority to subsidize health insurance for 7 million people who live in one of the 34 states using the federal health insurance exchange. Observers are watching Justice Anthony Kennedy closely, whose questions indicated that his vote is in play: if he sides with the Court’s four liberal justices to uphold ACA, the insurance subsidies will stand; if he sides with the Court’s other conservative justices, the federal insurance exchange will fall apart. The fate of people’s access to care is of particular concern in Florida, where over 1.6 million people obtain their health insurance through the federal exchange, and 93% of them receive subsidies.
In a reflection of the immense profits being made off of the commodification of health care, Justice Kennedy’s statements in support of the ACA’s insurance subsidies sentthe stocks of publicly traded hospitals, which are concentrated in Florida and Texas, soaring.
Health care spending is growing: New data from the Altarum Institute reveal thathealth care spending has grown dramatically in the first year of the Affordable Care Act, up 5% overall in 2014. While some of this growth can be attributed to increased utilization of care from people newly covered by insurance, much of the acceleration is associated with growing costs of prescription drugs and insurance. Drug spending was up 13%, and administration and health insurance expenditures increased by 11%. Health care spending now accounts for 18% of the U.S. gross domestic product. A national survey conducted in October reveals that 90% of people worry about how to pay for unexpected medical bills. This rate has held steady for the past three years, showing no indication that the ACA has done anything to increase people’s sense of security. One new study, meanwhile, analyzed insurers’ financial filings over the three years since the ACA first required insurers to spend 80-85% of premiums on actual medical care, and found that the law has done nothing to reduce the percentage of insurer expenditures on such things as administration, marketing and profits. A second study found that because of the U.S.’s multi-payer market-based insurance system, a quarter of hospitals’ budgets are consumed by administration, far more than in other countries.
Rural hospitals shutting down nationwide: Dozens of rural hospitals have been forced to close their doors since 2010 because of inadequate public funding. The Affordable Care Act reduced payments to hospitals for uninsured patients, yet as many states have refused to expand Medicaid, health care needs have not declined. The community of Belhaven, North Carolina, fought to oppose the closure of its local hospital, and is organizing a march from Belhaven to Washington, DC, from June 1 through June 13. Allies are invited to join. Stay tuned for more information in our April and May Bulletins.
New York State prisons deny women reproductive health care and reproductive decision-making: A powerful report from the Women in Prison Project of the Correctional Association of New York finds that women in New York State prisons are denied adequate access to quality reproductive healthcare. The report includes a set of recommendations for the State Legislature and the Governor, including reducing New York’s prison population, expanding funding for gender-specific, community-based alternative-to-incarceration and reentry programs, and building accountability mechanisms into laws to protect pregnant women and new mothers from shackling, solitary confinement, and other harmful forms of punishment. An article in Health and Human Rights Journal explains that perinatal shackling remains the standard in most U.S. states. The authors provide an overview of the laws and regulations governing perinatal shackling, and say that while a federal ban is very unlikely in the foreseeable future, state-based organizing efforts to advance the human rights and dignity of women are showing progress.
Ninety years after insulin was developed, many people with diabetes can’t afford it: As NPR reports, a new article in the New England Journal of Medicine explores the history of how drug companies have marketed and priced insulin to maximize their profits. This market-based approach to drug pricing leaves many people without access to the crucial drug. The marketization of insulin helps illuminate the problems that arise from treating health care as a commodity rather than a public good, and mirrors recent concerns over the marketization of breast milk, renewed proposals to marketize human kidneys, and, as renowned economist Jeffrey Sachs write, the profit-driven pricing of drugs at hundreds of times what they cost to produce. Overall, according to a new study, spending on prescription drugs went up 13% in 2014, and drug companies have been found to be systematically obfuscating the money they pay to doctors who prescribe their drugs. As Northeastern University law professor Brook Baker explains in a recent interview, when it comes to pharmaceuticals, human rights and proprietary intellectual property rights compete head to head, but while patents are fiercely protected by drug companies, human rights have no comparable enforcement mechanism built into the law. This means, he says, that human rights “lack teeth against many of the main perpetrators who are private actors – international corporations who do the most structural harm to access to medicines.” The solution, says Baker, lies in social movements that strategically deploy a human rights framework to advance structural change.
TPP threatens access to medicines: The U.S. government is currently in secret negotiations with 10 other governments of Pacific Rim countries on a proposed trade agreement called the Trans-Pacific Partnership (TPP). Leaked documents reveal that, among other things, the TPP would advance the profit interests of pharmaceutical companies by extending monopolies on drugs and thereby closing off people’s access to generic drugs, which would particularly harm those in poorer countries. The TPP would also require patenting of surgical, therapeutic, and diagnostic methods, which would create barriers for accessing these treatments. Check out this very helpful fact sheet from Doctors without Borders for more information on how the TPP would block access to medicine, and read calls for transparency and accountability from National Nurses United, doctors, Rev. Dr. William Barber II, economist Joseph Stiglitz, Senator Elizabeth Warren, andRepresentatives Raul M. Grijalva and Keith Ellison.
With billions in the bank, Blue Shield of California loses its state tax-exempt status: The Los Angeles Times reports that the giant private health insurer Blue Shield of California, which claims 3 million members and $13.6 billion in annual revenue, was quietly stripped of its nonprofit status by the State of California last summer. (The LA Times broke the story after a 7-month delay.) The insurer had been established as a “mutual benefit” nonprofit “dedicated to charitable, religious or public purposes,” according to California corporation law. This exempted Blue Shield from paying tens of millions of dollars in state taxes each year. (The insurer has donated $200 million to a foundation that it set up, about 5% of the $4.2 billion it holds in reserves. Of the $200 million, the foundation has given out $34 million in grants—less than 1% of Blue Shield’s reserves—to projects chosen by thefoundation’s board, half of whose members are Blue Shield executives.) After controversy over Blue Shields’ billions of dollars in reserves, large rate hikes, and exorbitant executive pay, the State conducted an audit, which resulted in its decision to require the company to pay state taxes. Blue Shield’s long-time public policy director resigned this month after 12 years at the company, saying it had been “shortchanging the public” for years; he is now leading a campaign to require the company to turn over its reserves to the state to finance public health programs.
Indiana’s Medicaid expansion imposes premiums and copays and creates inequitable access: In a dangerous development, Indiana will become the first stateto require a broad part of the poor population to pay premiums in order to be enrolled in Medicaid. People with incomes up to 133% of the federal poverty line will be required to pay up to 2% of their income as premiums. If they fail to pay those premiums and are just above the poverty line, they will be locked out of Medicaid (and thus health care access) for six months. If they are below the poverty line and fail to pay premiums, they will be charged co-pays and enrolled in a less comprehensive plan that will deny them vision, dental, and other health care that people above the poverty line have access to. By granting Indiana a waiver that essentially changes the nature of Medicaid – from facilitating access to care for poor people to obstructing their access – the federal government has set a precedent for further undermining this important public program. As the politics of Medicaid expansion continue to play out state by state, 22 states continue deny health care to millions of people in poverty. In a rare case of good news, however, Pennsylvania will fully transition by September from a plan much like Indiana’s that prioritized market ideology to a Medicaid expansion that prioritizes access to care.
Doctors speak out on why Black Lives Matter: In three opinion pieces in the New England Journal of Medicine and The Journal of the American Medical Association [1 2 3], doctors are speaking out about how racism hurts the health of Black people in the United States, and are calling for critical research on racism in health care; more hiring, promotion, training, and retention of staff of color in medicine; forming partnerships to meet patients’ needs; and more discussion within the medical professions of racial health disparities and implicit bias. For more, check out Healthcare NOW!’s readers’ guide to racial equity in health care.
