Hospital Closures
Nationwide Hospital Closures
Number of nationwide hospital closures in the last five years (2015-2019). [1] 73 of these hospitals were in rural areas and 62 in urban ones. [2] 1
Number of hospitals closed in 2019. 2
Number of hospitals closed in the first 3 months of 2020. 3
Number of rural hospitals currently at risk of closure because of lack of funding. [1, 2, 3] 196 are considered especially high risk. [4] 4
Percentage of rural hospitals at high financial risk that are considered “highly essential” to communities [1]. 64% of all rural hospitals are considered “essential” [2]. 5
Number of states in which 100% of high-risk hospitals are considered “highly essential” 6
Number of rural hospitals closed since 2005. 7
 Source: Cecil G. Sheps Center for Health Services Research
Source: Cecil G. Sheps Center for Health Services Research
Less likelihood of closure if a hospital is located in a state that has expanded Medicaid 8
Rate at which hospital closures accelerated after the Affordable Care Act went into effect (2013-2017, in comparison to all prior five-year periods) 9
Percentage of at-risk hospitals potentially eligible for federal funds under Medicare for All 10
1 [1]: Binkowski, Alison, Stephanie Cameron, Jeff Stensland, Dan Zabinski, Ledia Tabor, and Kim Neuman (December 2019). “Assessing
payment adequacy and updating payments: Hospital inpatient and outpatient services.” MedPAC.
[2]: Cecil G. Sheps Center for Health Services Research (2020). "170 Rural Hospital Closures: January 2005 – Present (128 since 2010).”
https://www.shepscenter.unc.edu/programs-projects/rural-health/rural-hospital-closures/.
http://www.medpac.gov/docs/default-source/default-document-library/hospital-december-2019-v5-public-no-rec-or-projmargin.pdf?sfvrsn=0.
2 MedPAC (March 2020). “Hospital Inpatient and Outpatient Services.” Report to the Congress: Medicare Payment Policy.
http://medpac.gov/docs/default-source/reports/mar20_medpac_ch3_sec.pdf?sfvrsn=0.
4 [1]: 430 according to Mosley, David (February 2019). "Rural Hospital Sustainability: New Analysis Shows Worsening Situation for
Rural Hospitals, Residents." Navigant. https://guidehouse.com/-/media/www/site/insights/healthcare/2019/navigant-rural-hospital-analysis-22019.pdf.
[2]: 453 according to Topchik, Michael (February 2020). "The Rural Health Safety Net Under Pressure: Rural Hospital Vulnerability."
The Chartis Center for Rural Health. https://www.ivantageindex.com/wp-content/uploads/2020/02/CCRH_VulnerabilityResearch_FiNAL-02.14.20.pdf.
[3]: 557 according to Thomas, Sharita (April 2019). "Geographic Variation in the 2019 Risk of Financial Distress among Rural
Hospitals" NC Rural Health Research Program. https://www.shepscenter.unc.edu/wp-content/uploads/dlm_uploads/2019/04/FDIGeo-1.pdf
[4]: Thomas (April 2019).
https://guidehouse.com/-/media/www/site/insights/healthcare/2019/navigant-rural-hospitalanalysis-22019.pdf
5 [1]: David, Daniel DeBehnke, Sarah Gaskell & Alven Weil (April 2020). “2020 Rural Hospital Sustainability Index Trends in Rural
Hospital Financial Viability, Community Essentiality, and Patient Outmigration.” Guidehouse. https://guidehouse.com/-
/media/www/site/insights/healthcare/2020/guidehouse-navigant-2020-rural-analysis.pdf.
[2]: Mosley (February 2019). See footnote 4.
https://guidehouse.com/- /media/www/site/insights/healthcare/2020/guidehouse-navigant-2020-rural-analysis.pdf.
9 United States Government Accountability Office (Aug. 29, 2018). "Rural Hospital Closures: Number and Characteristics of Affected Hospitals and Contributing Factors,” GAO-18-634.
https://www.gao.gov/products/GAO-18-634.
10 Palmquist, Ben (February 2019). “Human Rights Assessment of the Medicare for All Act of 2019.” Partners for Dignity & Rights.
https://dignityandrights.org/resources/m4all2019/
Lack of Hospital Beds During COVID-19
Projected shortage of hospital beds during the COVID-19 pandemic in a 6-month period 11
Number of hospital beds lost to hospital closures since 2005 in rural areas alone 12
Number of hospital beds lost to hospital closures in the first 3 months of 2020 alone 13
Percentage of counties with no ICU beds. These counties are home to 18 million people. 14
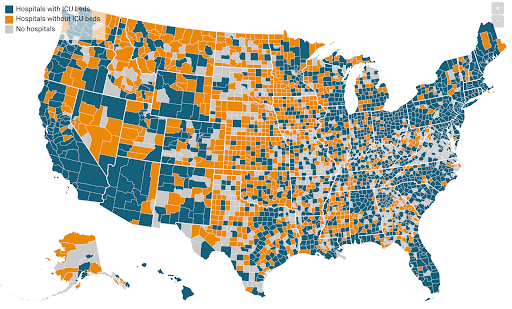 Source: Kaiser Family Foundation
Source: Kaiser Family Foundation
Number of people who live in counties with no hospitals 15
Number of people living more than 30 minutes from the nearest hospital. California, Florida, Arizona and Washington each have more than half a million people over 30 minutes away. 16
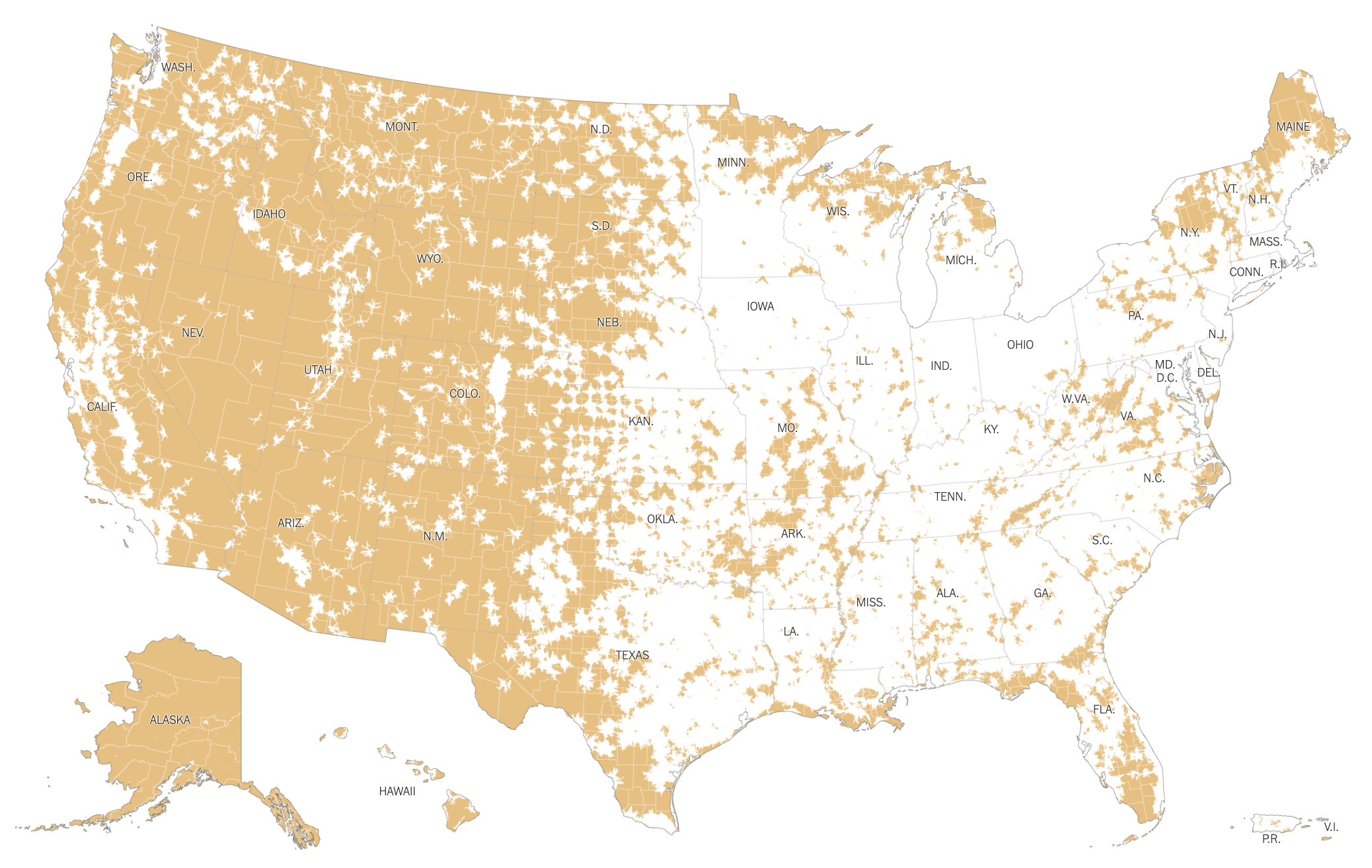 Source: New York Times
Source: New York Times
Number of hospital beds for every 1,000 people in 1960 and 2013 17
11 Tsai, Thomas (Mar. 17, 2020). "American Hospital Capacity and Projected Need for COVID-19 Patient Care." Health Affairs.
https://www.healthaffairs.org/do/10.1377/hblog20200317.457910/full/.
12 Cecil G. Sheps Center (2020). See footnote 1.
https://www.shepscenter.unc.edu/programs-projects/rural-health/rural-hospital-closures/.
14 Schulte, Fred, Elizabeth Lucas, Jordan Rau, Liz Szabo & Jay Hancock (March 20, 2020). "Millions Of Older Americans Live In Counties With No ICU Beds As Pandemic Intensifies." Kaiser Family Foundation.
https://khn.org/news/as-coronavirus-spreads-widely-millions-of-older-americans-live-in-counties-with-no-icu-beds/
16 Koeze, Ella, Jugal K. Patel and Anjali Singhvi (April 26, 2020). "Where Americans Live Far From the Emergency Room." New York Times.
https://www.nytimes.com/interactive/2020/04/26/us/us-hospital-access-coronavirus.html
17 The World Bank. "Hospital beds (per 1,000 people) – United States."
https://data.worldbank.org/indicator/SH.MED.BEDS.ZS?end=2013&locations=US&start=1960&view=chart.
Disparities in Geography, Race, Class, Gender
Percentage of rural hospital closures that took place in states that did not expand Medicaid 18
Percentage of rural hospital closures that have taken place in the South 19
Number of rural hospitals at risk in Texas alone (followed by Kansas with 31, Oklahoma with 28, Mississippi with 27, Missouri with 26) 20
Percentage of vulnerable hospitals located in rural areas 21
Increased odds of an emergency department closing for every 10% increase in the Black population 22
Odds of Black-majority census tracts in Los Angeles and Chicago of being located in a trauma center desert relative to White-majority tracts 23
Fraction of the 230 hospitals opened across the country since 2000 opened in wealthier areas 24
Percentage of rural women and transgender people who have to travel more than 30 miles for neonatal care 25
Counties in the U.S. without a known abortion clinic 26
18 Wick, Colin (January 2, 2020). "The Case for Nationalizing Rural Hospitals." Data for Progress.
https://www.dataforprogress.org/memos/the-case-for-nationalizing-rural-hospitals.
19 Ibid. Thomas (April 19) from footnote 3 estimates 73%. In addition, nine out of ten states with the highest median uncompensated care as a percentage of operating expense are located in the South. See Garcia, Krystal (June 2018). "Geographic Variation in Uncompensated Care Between Rural and Urban Hospitals." Rural Health Research Gateway.
https://www.ruralhealthresearch.org/publications/1186.
22 Hsia, Renee (Nov. 16, 2011). "System Level Health Disparities in California Emergency Departments: Minorities and Medicaid Patients are at Higher Risk of Losing Their EDs.” U.S. National Library of Medicine National Institutes of Health.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4636219/.
23 Tung, Elizabeth L., David A. Hampton, Marynia Kolak, et al. (March 8, 2019). “Race/Ethnicity and Geographic Access to Urban Trauma Care.” JAMA Netw Open. 2019;2(3):e190138. doi:10.1001/jamanetworkopen.2019.0138.
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2727264.
24 Thomas, Lillian (June 14, 2014). "Poor Health/A special report: How we did it." Pittsburgh Post-Gazette.
https://www.postgazette.com/news/health/2014/06/13/Poor-Health-A-special-report-How-we-did-it/stories/201406130157
25 P, Hung (June 2018). "Rural-urban differences in access to hospital obstetric and neonatal care: how far is the closest one?" PubMed.
https://www.ncbi.nlm.nih.gov/pubmed/29453436.
26 Jones, Rachel (2019). "Abortion Incidence and Service Availability in the United States, 2017." Guttmacher Institute.
https://www.guttmacher.org/report/abortion-incidence-service-availability-us-2017.
Health and Economic Impacts
Fewer medical visits that would occur with widespread (673) hospital closures 27
Number of health care and community jobs that would be lost to widespread rural hospital closures 28
Loss in GDP over 10 years due to projected widespread hospital closures 29
Difference in mortality rates between rural and urban areas (2015) 30
Rate at which the difference in mortality between rural and urban areas has increased over the last fifteen years (18% mortality disparity in 2015, up from 6% in 2000) 31
Average decline in a county’s per-capita income when its only hospital shuts down 32
27 iVantage Health Analytics (2016). "Rural Relevance – Vulnerability to Value."
https://www.chartis.com/resources/files/INDEX_2016_Rural_Relevance_Study_FINAL_Formatted_02_08_16.pdf.
30 Hoffman, Abby (Aug. 2017). "Regional Differences in Rural and Urban Mortality Trends." NC Rural Health Research Program.
https://www.shepscenter.unc.edu/wp-content/uploads/dlm_uploads/2017/08/Regional-Differences-in-Urban-and-Rural-MortalityTrends.pdf.
32 Holmes, George (April 2006). "The effect of rural hospital closures on community economic health." Health Services Research.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1702512/.
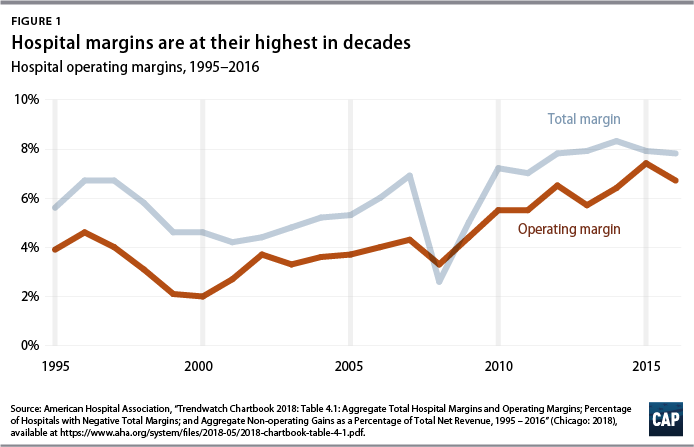
Hospital Ownership, Profitability and Closures
Portion of rural hospitals considered unprofitable 33
Odds of a for-profit rural hospital being in financial distress relative to a non-profit hospital 34
Percentage increase in the share of hospitals owned by for-profit companies from 1999 to 2018 35
Percentage of hospital revenue paid by Medicare and Medicaid (59.3%) 36
Percentage of hospital revenue paid by private payers 37
Amount the State of Pennsylvania will pay private equity firm Cerberus Capital Management to keep Easton Hospital open for three months Cerberus threatened closure on March 27 in the midst of the pandemic 39
33 Pink, George, Kristie Thompson, Ann Howard & Mark Holmes (March 2018). "Geographic Variation in the 2016 Profitability of
Urban and Rural Hospitals." NC Rural Health Research Program.
https://www.shepscenter.unc.edu/wpcontent/uploads/dlm_uploads/2018/03/Geographic-Variation-2016-Profitability-of-Rural-Hospitals.pdf.
34 McCay, Dennis (Spring 2019). "A Case Study: Organizational and Environmental Factors Associated with Alabama Rural
Hospitals’ Reported Levels of Financial Distress." Journal of Health Care Finance.
http://healthfinancejournal.com/index.php/johcf/article/view/177.
35 Kaiser Family Foundation (2018). "Hospitals by Ownership Type.”.
https://www.kff.org/other/state-indicator/hospitals-byownership/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D.
36 American Hospital Association cited in Gee, Emily (June 26, 2019). “The High Price of Hospital Care.” Center for American
Progress.
https://www.americanprogress.org/issues/healthcare/reports/2019/06/26/471464/high-price-hospital-care/.
39 Batt, Rosemary & Eileen Appelbaum (April 2, 2020). "Hospital Bailouts Begin—for Those Owned by Private Equity Firms." The
American Prospect.
https://prospect.org/economy/hospital-bailouts-begin-for-those-owned-by-private-equity-firms/.